Birth Control
Non-Hormonal Birth Control
Non-hormonal contraceptives prevent contraception by physically preventing sperm from meeting an egg. This can be done by barrier methods like condoms and diaphragms, by killing sperm with spermicide or copper, or by permanent sterilization.
Diaphragm
-
A diaphragm is a soft silicone “cup” inserted into the vagina before sex.
-
The diaphragm covers the cervix (the opening to the uterus) and prevents sperm from entering. The diaphragm is most effective when used with Spermicide.
-
Fitted diaphragms can be obtained from your doctor with a prescription. “One size” diaphragms can be purchased at a pharmacy without a prescription. They cost up to $15-$75.
-
Inserting the diaphragm
Check the diaphragm for holes, cracks and tears by holding it up to the light. Check the expiry on the gel.
Empty your bladder before you put your diaphragm in to prevent a bladder infection.
Wash your hands with soap and water for at least 20 seconds.
Put spermicidal or acid buffering gel inside the diaphragm. The gel needs to be on the side of the diaphragm that will be right next to the cervix.
Put your diaphragm in up to 2 hours before you have sex.
Lie down, squat, or raise one leg on a chair or toilet.
Squeeze the rim together and push the diaphragm into the vagina, as far as it will go towards the back bone.
When the diaphragm is most of the way in, let go of it and tuck the front edge of the diaphragm up behind the pubic bone.
Make sure you can find your cervix (it feels like the tip of your nose) through the diaphragm.
If your diaphragm is in the right place, you should not feel it. If it isn’t comfortable, it’s likely not in the right place. Take it out and try again.
Removing the diaphragm
It must stay in for at least 6 hours after sex. Don’t keep it in for more than 24 hours.
Wash your hands with soap and water for at least 20 seconds.
Hook your finger under the rim and gently pull the diaphragm down and out to avoid damaging it.
After each use, wash your diaphragm with mild, unscented soap and warm water. Rinse and dry it completely.
Store it in a cool, dry place.
Spermicide
-
Spermicide is usually a cream, foam, or gel applied inside the vagina or inside a diaphragm before sex. The only form of spermicide available in Canada is ContraGel, a jelly that contains lactic acid.
-
Spermicide kills sperm on contact. It works best when used with another barrier method, like diaphragms or condoms.
-
Spermicide is available at most pharmacies without a prescription. They cost $15-$20.
-
Always use vaginal spermicides with another form of birth control (e.g., condoms).
Always use the right amount of spermicide (see package directions).
Before using a spermicide, check the expiry date on the package. Don’t use products that are expired.
Put the spermicide up high in the vagina to cover the cervix.
With some spermicide products, you have to wait before you have sex (see package directions).
You have to put spermicide in each time you have sex.
Don’t rinse or douche for at least 6 hours after having sex (douching is not ever recommended).
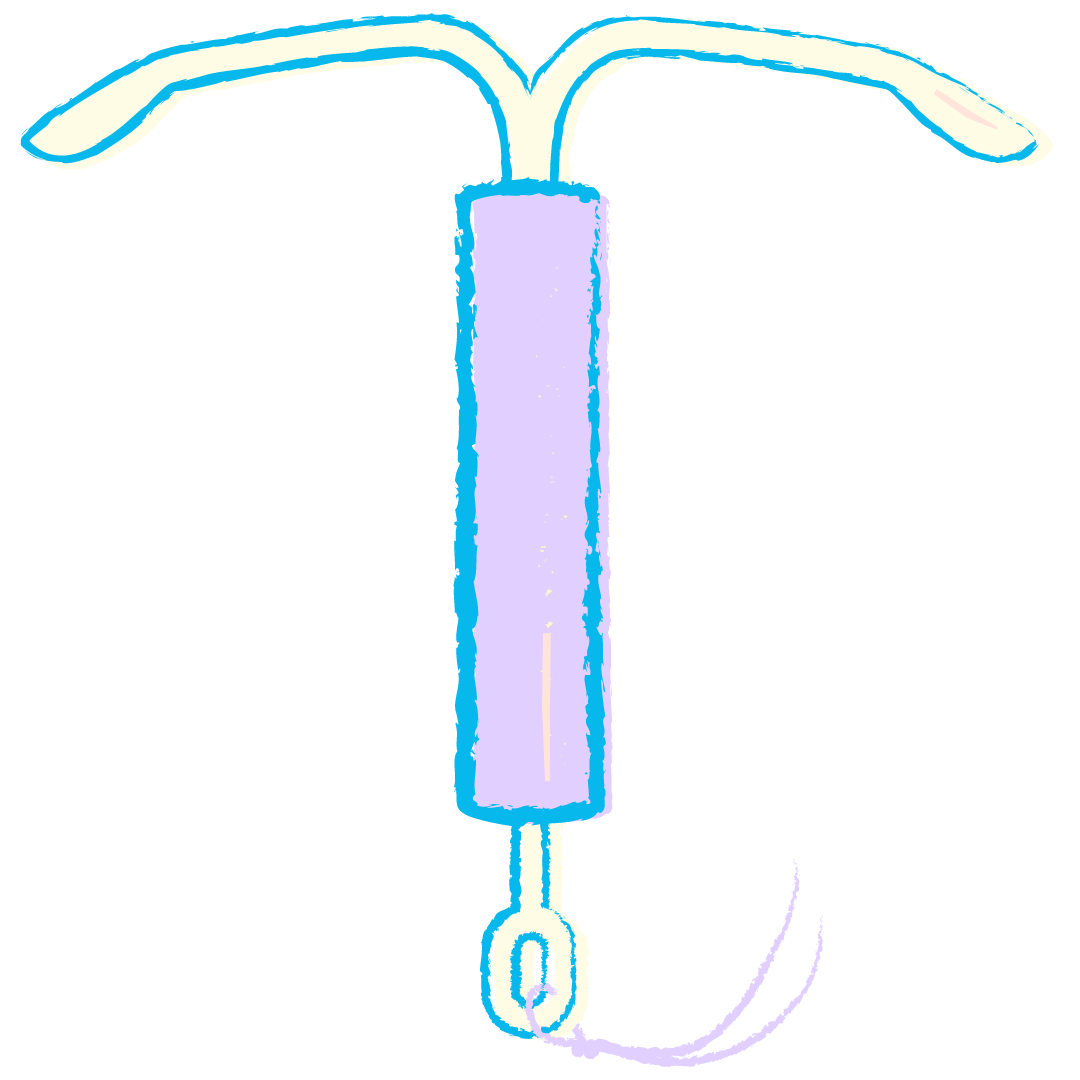
Copper IUD
-
A copper IUD is a T-shaped instrument inserted into the uterus.
-
The copper of the IUD is a type of spermicide, meaning it kills sperm on contact. Based on doctors' recommendations, copper IUDs can be used for 3-10 years or longer.
-
You will need a prescription for a copper IUD and an appointment to have it inserted. They cost around $175-$350.
-
Once inserted, you will not have to do anything else. It is recommended to use another form of birth control for 2 weeks after the insertion. After your 3-10 years are completed, you will need to make an appointment to have the IUD removed.
Surgical Sterilization
-
Tubal Ligation closes the fallopian tubes (female).
A Vasectomy closes the vas deferens (male).
Both are considered permanent forms of birth control. However, a clamp vasectomy has the highest successful reversal rate.
-
A tubal ligation may be performed by cauterizing, cutting, clipping, or removing the fallopian tubes so eggs or ovum are not able to get to the uterus to be fertilized by sperm. This does not impact the menstrual cycle.
A vasectomy may be performed by cutting on clamping the vas deferens so sperm cannot move from the scrotum through the penis. A vasectomy does not change ejaculation.
-
Both tubal ligations and vasectomies require a doctor to perform. AHS covers the cost of both procedures with an Alberta Health Card.
-
After the procedure, you will not have to do anything else, as surgical sterilization is permanent.
Hormonal Birth Control
Hormonal Birth Control is highly effective and safe for most people. Hormonal contraceptives use estrogen and progestin, or progestin-only (both are produced naturally in your body). You may have to try a variety of different types to find the best one for your body and lifestyle.
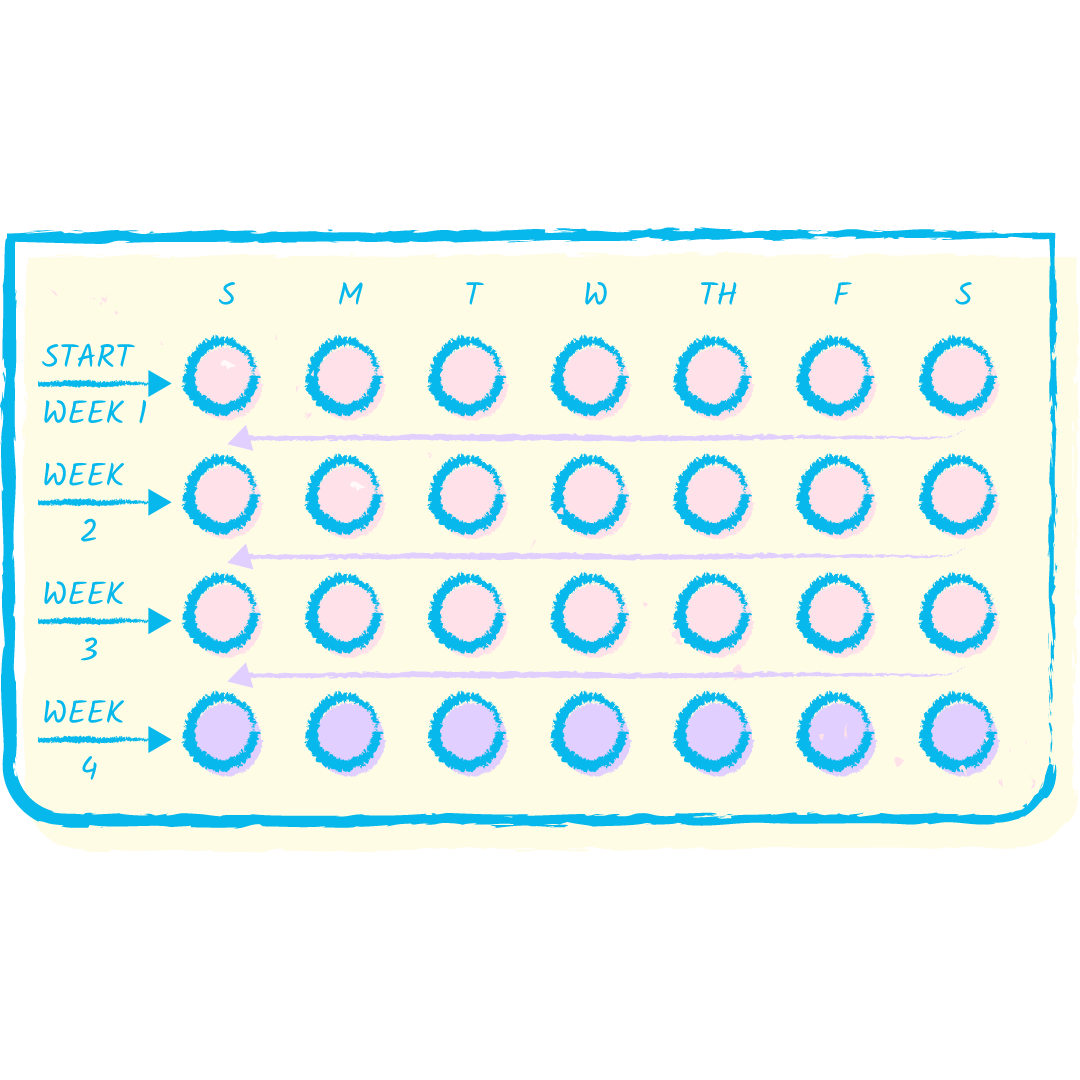
The Pill
-
A combination (estrogen and progestin) or progestin-only pill you take by mouth every day.
-
The hormones in the pills prevent the ovaries from releasing an egg, so there is nothing to be fertilized by sperm.
-
You will need a prescription to get birth control pills. 1 pack (1 month) costs between $0-$50, depending on your insurance or assistance programs.
-
To use a 28‑day pack:
Take 1 pill each day at the same time. The 28‑day packages come in different ways:
first 21 pills have hormones, and the last 7 pills are hormone‑free
first 24 pills have hormones, and the last 4 pills are hormone‑free
first 26 pills have hormones, and the last 2 pills are hormone‑free
You’ll usually get your period 2 to 3 days after starting the hormone‑free pills. You’re still protected from pregnancy during this time.
When the pack is done, start a new pack the next day. Always start your new pack of pills on time, even if your period hasn’t ended. Your period should stop in a few days.
If you don’t have a period, start your new pill pack and see your healthcare provider.
To use a 21-day pack:
Take 1 pill each day at the same time for 21 days.
When the pack is done, wait 7 days before starting a new one. You’ll get your period when you aren’t taking pills (hormone‑free days). You’re still protected from pregnancy during this time.
The hormone‑free days must not be longer than 7 days. At the end of the hormone‑free days, start a new pack. Always start your new pack of pills on time, even if your period hasn’t ended. Your period should stop in a few days.
If you don’t have a period, start your new pill pack and see your healthcare provider.
If you miss a day:
Take 1 pill right away (this might mean you take 2 pills on the same day).
Continue to take 1 pill every day until the end of the pack.
Use a backup form of birth control (e.g., condoms, abstinence) for 7 days.
Get emergency contraception as soon as possible if your backup form of birth control fails (e.g., condom breaks) or you’ve had unprotected sex in the last 5 days.
The Patch
-
A birth control patch is like a bandaid worn on the skin for 1 whole week.
-
The sticky part contains estrogen and progestin that are released into the skin to prevent the ovaries from releasing an egg, so there is nothing to be fertilized by sperm.
-
You will need a prescription to get birth control patches. A pack contains 3 patches (1 month’s worth) and costs between $0-$150, depending on your insurance or assistance programs.
-
Only use 1 patch at a time. Put the patch on clean, dry skin on your upper buttocks, upper outer arm, abdomen, or upper body. Put each new patch in a different place (e.g., change between the right and left sides) to keep your skin from getting irritated.
Press down firmly on the patch with the palm of your hand for 10 seconds to make sure the edges stick well. If a patch isn’t sticking, try to put it on again in a different place. If it won’t stick, remove it and put a new patch on immediately. Talk to your pharmacist or healthcare provider if you need a replacement patch.
If your skin gets irritated, take the patch off and put a new one on in another place (your patch change day stays the same).
Leave the patch on during activities (e.g., exercise, shower, swim)
Be aware that used patches still contain hormones. After removing a patch, fold it inwards so it sticks to itself and put it in a garbage that is out of a child’s or pet’s reach.
Store your patches at room temperature (never put them in your fridge or freezer)
When you use the patch, don’t:
use any bath oil, body wash, lotion, or powder on the area where you will put your new patch
put the patch on your breasts
put the patch on skin that is red, cut, or scratched
use bandages or tape to hold the patch in place, as this affects how the hormones are absorbed
Your patch change day is the day of the week that you put your patch on. Always use a new patch on the same day of the week, at the same time.
You wear a patch for 1 week at a time. A new patch is put on each week for a 3-week cycle. You don’t put a patch on during week 4 (hormone-free days). This is when you get your period.
Start your next cycle by putting on a new patch after the hormone-free days. Put on a new patch, even if you still have your period. Your period should stop in a few days. If you haven’t had your period, put the patch on and call your healthcare provider.
Never have the patch off for more than 7 days in a row.
Nuvaring
-
A clear plastic (not latex) ring inserted into the vagina.
-
The ring contains estrogen and progestin that are released into the vagina to prevent the ovaries from releasing an egg, so there is nothing to be fertilized by sperm.
-
You will need a prescription to get birth control rings. A pack contains 1 ring (1 month’s worth) and costs between $0-$30, depending on your insurance or assistance programs.
-
Put the ring in your vagina. Leave the ring in for 3 weeks (21 days). After 3 weeks, take the ring out. You’ll start your 7 hormone-free days. You’ll get your period when you aren’t wearing the ring. You’re still protected from pregnancy during this time.
After your 7 hormone-free days, always put in a new ring. Even if you still have your period, you need to put a new ring in. You can use a tampon when you have the ring in. If you haven’t had your period, put a new ring in and contact your health care provider.
Putting the ring in
Wash your hands. Get into a comfortable position (e.g., standing with one foot up on a chair).
Squeeze the ring between your thumb and finger. Gently push it up into your vagina. It doesn’t matter how the ring is placed, as long as it’s high enough that it won’t fall out. If it feels uncomfortable, the ring might not be up far enough. Use your finger to push it further up. The ring can’t get lost in your vagina or be pushed in too far.
Taking the ring out
Wash your hands.
Hook your finger under the rim and pull the ring down and out. Throw it in the garbage, away from children and pets, because it still contains hormones.
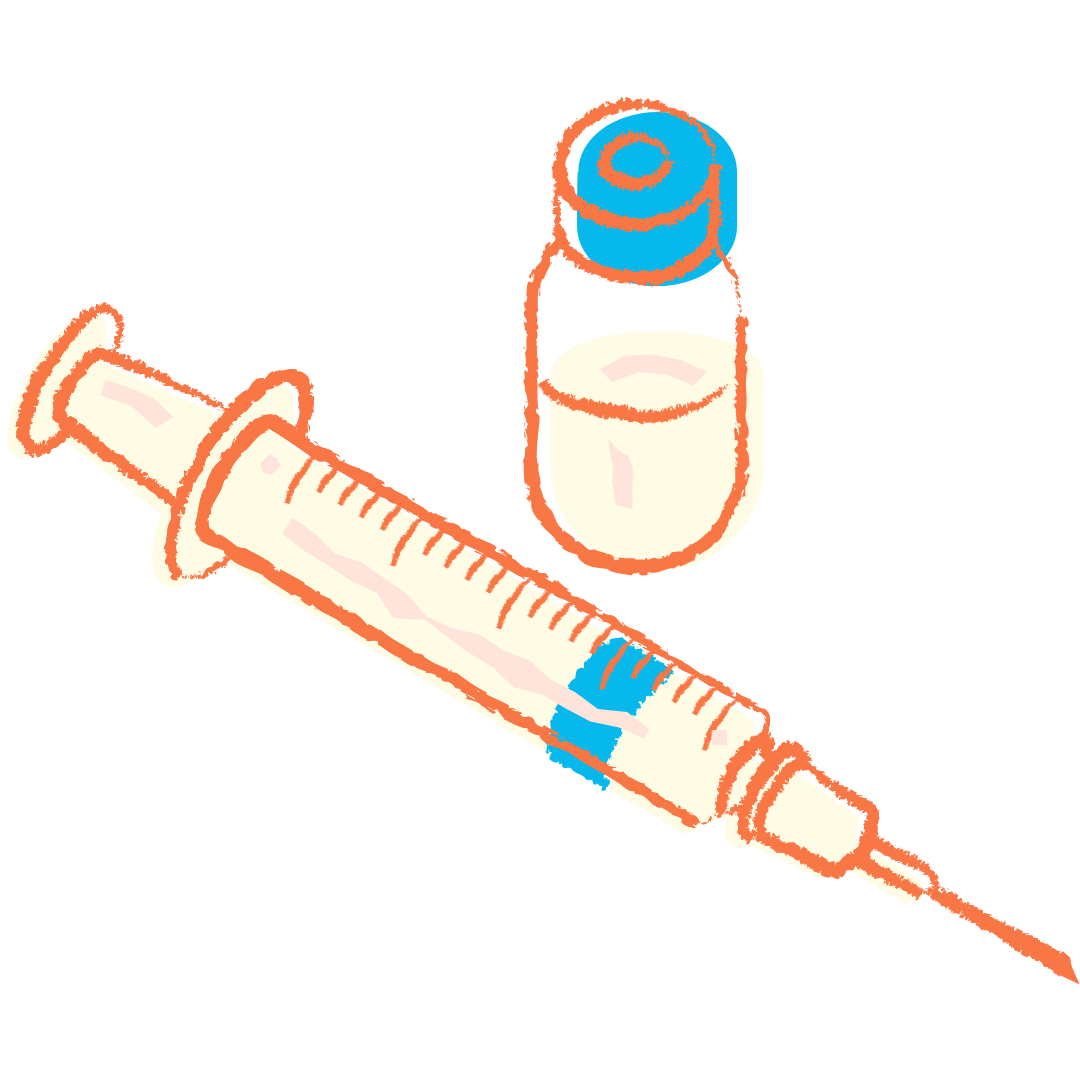
Depo-Provera
-
An injection given in the arm or buttocks every 12-13 weeks (about 3 months).
-
The shot contains progestin that is released into the body to prevent the ovaries from releasing an egg, so there is nothing to be fertilized by sperm.
-
You will need a prescription to get the shot. 1 shot (3 months’ worth) costs between $0-$150, depending on your insurance or assistance programs.
-
The birth control injection is given by a health care provider.
There are different ways to start the injection. If you get your first injection:
During the first 5 days of your period, it takes 24 hours to become effective. Consider using an extra form of birth control (e.g., condoms) during this time
at any other time, you need to use an extra form of birth control (e.g., condoms) for 7 days
Nexplanon
-
A thin plastic tube (about 4cm or 1.5”) inserted just below the skin of the upper arm.
-
The implant contains progestin that is released into the body to prevent the ovaries from releasing an egg, so there is nothing to be fertilized by sperm.
-
You will need a prescription to get the implant. 1 implant (lasts for 3 years) costs between $0-$350, depending on your insurance or assistance programs.
-
Your healthcare provider will numb your skin and put the implant just under the skin of your upper arm. This takes a few minutes. When the implant is in place, you’ll have a dressing and an adhesive (sticky) bandage over the area. Your healthcare provider will tell you when you can take them off.
You probably can’t see your implant, but you can feel it if you touch the skin over it. Your healthcare provider will show you how to feel your implant.
If you get your implant on day 1 to 5 of your period, it works right away. If you get it any other day, use an extra form of birth control (such as condoms) for 7 days.
Hormonal IUD
-
A T-shaped instrument inserted into the uterus.
-
The implant contains estrogen and progestin that are released into the body to prevent the ovaries from releasing an egg, so there is nothing to be fertilized by sperm.
-
You will need a prescription to get an IUD. 1 IUD (lasts for 3-10 years) costs between $0-$450, depending on your insurance or assistance programs.
-
Once inserted, you will not have to do anything else. It is recommended to use another form of birth control for 2 weeks after the insertion. After your 3-10 years are completed, you will need to make an appointment to have the IUD removed.